So you’ve read Part 1, and you’re back for more? Great! Read on… If not…go read it now, or watch the video below for a crash course!
(Actually, watch the video anyway…there are a few updates I’ll discuss in more detail below…)
The Congenitally Crooked Neck from Foundations of Soundness on Vimeo.
How do all of our findings on observation, palpation and dissection relate to each other?
Muscle trouble: Longus colli
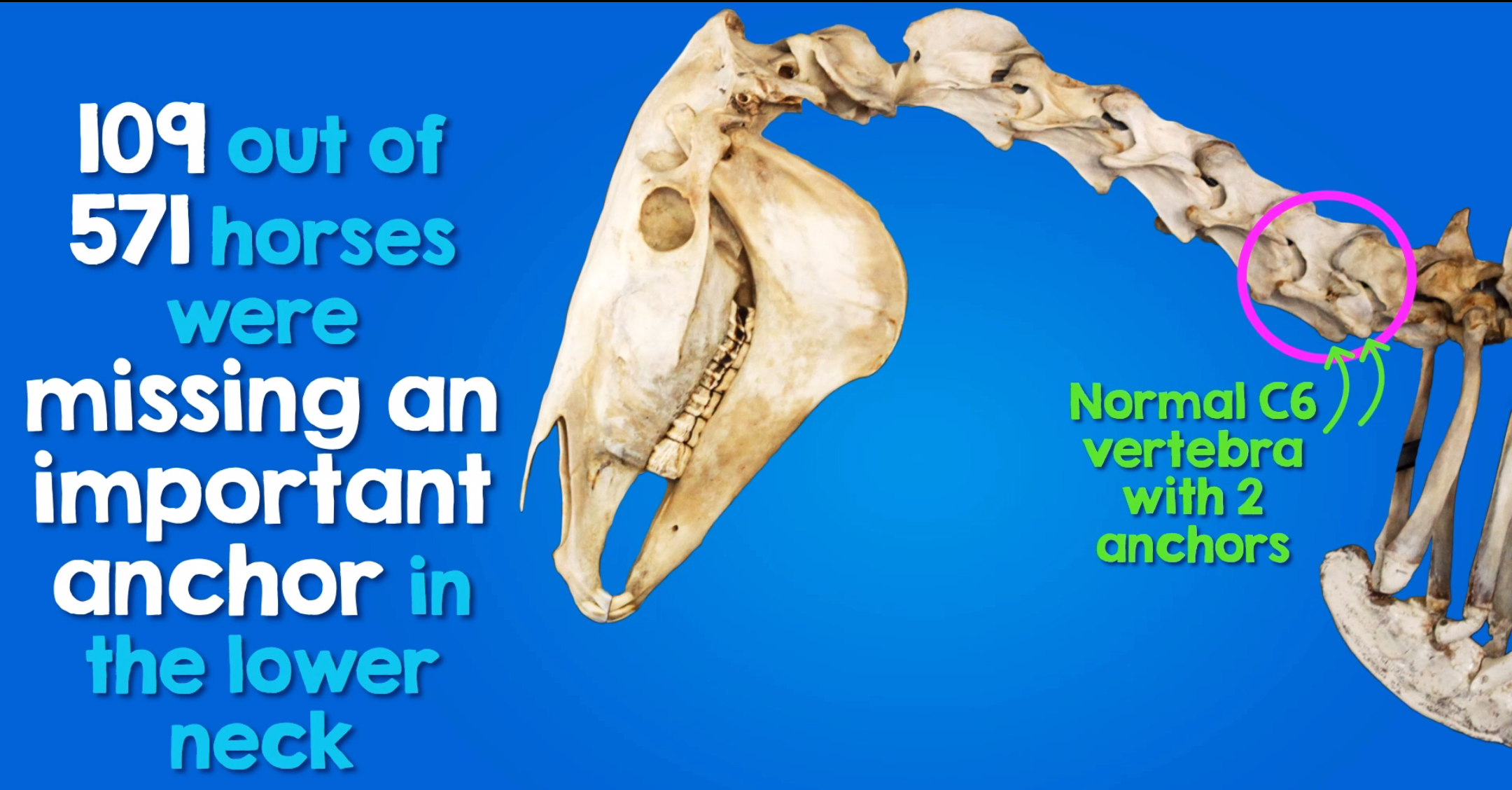
Responsible for flexing and fixing the caudal cervical vertebrae, m. longus colli normally attaches to the process that goes missing in the congenital malformations of C6 and C7. When this anchor is missing from C6, m. longus colli is forced to latch on anywhere it can. In a unilaterally affected horse, we now have asymmetrically acting muscles…but that’s not all.
M. longus colli, as the deepest muscle supporting the underside of the cervical vertebrae, is a richly innervated postural—or cybernetic—muscle with a huge role in proprioception. As Denoix describes:
“Proprioceptors transmit information on the muscles’ state of tension to the brain via reflex paths. Their proximity to the joints, the wealth of postural information they contain and the variety of possible responses which they are capable of are the features which distinguish them from the gymnastic muscles.
It is the cybernetic muscles which respond to the rider’s subtler commands.”
Was it possible that the brain wasn’t getting the correct feedback, with scoliosis and altered forelimb stance becoming the horse’s version of ‘normal’? This is part of the question addressed in this research study published in 2015…
Aside from the aspects addressed in the paper, I had to wonder… Could disorganised and dysfunctional attachment of m. longus colli (and m. scalenus too, in some horses with concurrent rib malformations) explain why riders describe these horses as being so blocked, crooked and unresponsive through the base of the neck?
As a classically trained violinist with a fair chunk of experience in the Alexander Technique during my formative years, Denoix’s perspective on the role of postural and neuromotor control in training the young horse (which you can read more about in Physical Therapy & Massage For The Horse) triggered a line of thinking which would steer my research, study and rehabilitation work down a more interesting path than I ever imagined. We’ll get to that…possibly not all of it in this piece, though!
Asymmetry creates more asymmetry
I get it. The horse is a huge animal, and it’s hard to fathom how such a small structural asymmetry could have such a big impact. But think about it… The bones are in a critical area for postural support of the whole body, and the horse is starting its life with asymmetry already present. The uneven muscle attachments might not seem like a big deal, but what about their effect on the bones in the growing horse, not to mention over the rest of their lifespan? As Dr Kerry Ridgway once put it:
“Asymmetry is dysfunction―dysfunction produces incorrect and compensated movement―pathology is the inevitable consequence.” (Ridgway, 2007, p. 174)
But how does this malformation actually affect the rest of the body?
Via the fascia…it’s all linked!
Myofascial meridians and dysfunction in the Deep Ventral Line
Let’s rewind to the start of 2014 for a moment…
I was sitting in one of the first lectures at Dr Kerry Ridgway’s fascia-based acupressure course, when the implications of new research mapping the equine equivalent of Myers’ ‘Anatomy Trains’ struck me like a lightning bolt.
You see, of the eight myofascial kinetic lines Schultz and Elbrønd had recently explored in the horse, the structure and function of the Deep Ventral Line (DVL) provided an anatomical explanation for some of the most common biomechanical issues we were observing in horses with the malformation.

Travelling up the horse’s hindleg into the pelvis (via the deep digital flexor and medial thigh muscles), the DVL splits into three sections, with the lower two of these encompassing the abdominal wall, diaphragm and ventral structures as far as the skull, mandible and hyoid apparatus.
The most dorsal pathway?
It passes along the ventral surface of the spinal column, via none other than m. longus colli, before reaching the skull. It is also believed to have an important relationship with the craniosacral system.

Adapted from Anatomy Trains: Myofascial meridians for movement and manual therapists (Myers, 2013b, pp. 184, 186) and Schultz and Elbrønd’s description of myofascial kinetic lines dissected in the horse (Schultz & Elbrønd, 2014).
But that wasn’t all. As I considered how myofascial dysfunction might snowball through the DVL from the altered attachments of m. longus colli at C6 and C7, many of the more abstract characteristics I had observed in affected horses began to make sense; I could suddenly put my finger on what I almost thought I had imagined.
I began getting in tune with the human equivalent in my own body to help build a mental picture of how this chain was affecting the horses I was working with, and how I could influence it through bodywork (and through training…but more on that in the next part of this series!), and I ordered the conference proceedings to chew over some of the clinical signs attributed to DVL dysfunction.
Reflecting the structures comprising the DVL and the forces potentially exerted on them, these symptoms were things like: stiffness potentially affecting the occipital to sacral regions of the spine, restricted forelimb range of motion “as if there was a board in front of the shoulders” (Due, 2014, p. 63), tripping in the forelimbs, rib pain, diaphragm dysfunction or hyoid pain, among others.
Consider this: while we often hear about tight, restricted or stuck-down and frozen fascia, the impact of fascial dysfunction is not solely mechanical. Fascia is a richly innervated neurosensory organ, and mechanical restrictions can have a profound impact on proprioception and neuromotor control (Schleip, 2003). As Peters and Rombach put it:
“Osseous degenerative lesions in the cervical vertebrae are not the start of a problem but instead represent an end stage of slow-onset joint failure secondary to inadequate neuromuscular control of the perivertebral muscles” (Peters & Rombach, 2015, p. 98).
What role do you think the DVL might play in this process? For my money, it’s a pretty big one. What’s more, DVL dysfunction—particularly originating from the cervicothoracic junction—will almost inevitably manifest in the horse’s connection to the rider’s hand via the reins, and may be obvious to the rider long before any clinical signs emerge.
So what did horses with the malformation have to say about the Deep Ventral Line connection?
Although evaluation of DVL dysfunction was conducted retrospectively for my thesis (e.g. by evaluating existing observational data against parameters relating to DVL dysfunction), all but one of the horses were evaluated via palpation after originally forming the hypothesis of a relationship between the DVL and the functional implications of these malformations; this included later assessments of my own horse prior to confirming his malformation post-mortem. The exception was one warmblood mare, my 2013 observations of whom triggered this hypothesis when I was initially studying the DVL in the following months.
For the seven horses in the study, manifestations of DVL dysfunction identified included:
- neck dysfunction (n=7)
- head tilt ± lateral C0/C1 restriction (n=7)
- restricted forelimb ROM (n=7)
- forelimb stumbling (n=6)
- back/rib pain or hypomobility (n=7)
- lumbar/sacral/pelvic restriction (n=7)
- restriction or resistance to caudal stretching of the hindlimb (n=6)
While only one horse exhibited clinical respiratory dysfunction, three additional horses displayed a ‘heave line’ associated with overuse of the external abdominal obliques, which potentially suggests diaphragm, pleural or other respiratory dysfunction.
One horse owner described the neck dysfunction and lateral atlanto-occipital restriction present in the warmblood mare as follows:
“When she turned her head to look behind her, she seemed unable to bring her neck around in a smooth curve but had to cock her head, with her neck remaining fairly straight and stiff with the poll at wither level.”
The strongest evidence of DVL dysfunction in these horses was the rotational torsion evident throughout the chain or at multiple sites when palpating fascial tension…which was mirrored at the skeletal level.

But the most interesting revelation about the DVL’s influence in horses with the malformation came when I evaluated footage and historic observations of the horses under saddle (including commentary from owners and trainers, and personal observations made in the saddle and/or from the sidelines) against the qualities of the German Training Scale, and screened all available data for manifestations of lameness under saddle as described by Dyson. Why? Because even though the ridden observations didn’t target the DVL, it was heavily implicated in the findings…but more on that later.
Connecting the dots from outside to inside… Can we predict it?
In each horse I personally evaluated, the individual features of the C6 and C7 malformations corresponded with the appearance of the cervicothoracic junction and the characteristics of palpation findings. Moreover, both horses referred for clinical examination and cervical radiograph studies were correctly predicted to exhibit bilateral malformations, while the format of the anomaly was clearly identifiable via manual palpation in the foal euthanised in utero that mirrored the form her mother was subsequently confirmed to exhibit.
So how did I pick them?
Back in 2014, after familiarising many of us with some of the signs through her dissection and biomechanics workshops, Sharon May-Davis put together a “subjective checklist” for students of the Australian College of Equine Podiotherapy. Given a big barrier to the progress of Sharon’s research in this area was the perceived subjectivity, it’s pretty encouraging to note that the findings based on visual and palpable markers in my little group mirrored the list articulated by Sharon, who found that these red flags assisted in distinguishing suspect horses in a day-to-day setting.
Indeed, these markers enabled me to repeatedly predict the presence of the malformation correctly, including a left, right or bilateral format, the latter being those horses for whom I could not make a clear left or right prediction.
You know what else is very telling?
The informal publication of these markers was within supporting materials for Sharon’s presentation at a conference conducted for past and present students of the Australian College of Equine Podiotherapy, during which three practitioners including myself presented observations made while working alongside—and underneath—horses later confirmed to exhibit the anomaly, with emphasis on the difficulties we encountered from an occupational health and safety perspective due to balance and pain-related challenges in handling these horses.
Quantifying these clues does more than highlight the value of carefully cataloguing subjective findings when faced with an unknown phenomenon and an absence of suitable diagnostic pigeonholes… It also squarely challenges the argument for a benign clinical character, based on the ability to identify horses exhibiting the anomaly according to markers that distinguish them from ‘normal’ horses, regardless of veterinary findings.
In other words, we could predict the presence of the anomaly because we perceived these horses as abnormal.
Indeed, many of the seemingly obscure findings I described to my peers in 2014, including the relationship to the Deep Ventral Line (DVL), evolved into significant parts of my Masters research project, as I began noticing similar patterns in other horses and building a mental list of candidates for a future study rigorously investigating clinical characteristics based on the work I presented in my thesis. Three of those horses I had mentally tagged ultimately contributed to my thesis posthumously.
Neck pain, myofascial chain dysfunction and the relationship to postural and training observations
Neck pain and DVL dysfunction are somewhat unsurprising findings considering the structures involved in these malformations and their far-reaching anatomical connections, and the functional impact on vertebral, postural and sensory dynamics in horses showing any combination of these signs should not be underestimated.
However, one might predict that we would also find these issues in many other horses; especially those involved in high-impact disciplines, those suffering from post-injury or chronic postural dysfunction, and in particular, horses subjected to biomechanically questionable training techniques such as rollkur/low, deep and round (LDR).
The horses with the congenital malformations of C6 and C7 were a bit different though: the neck dysfunction noted in the presence of the malformation was characterised by fascial torsion through the Deep Ventral Line, whether or not they also exhibited muscular problems I frequently find in other horses I don’t suspect have the malformation. But that’s not all… This pattern was also reflected in the type of crookedness displayed in the ridden horse, and highlights a significant challenge in training these horses for comfort rather than compounding their pain.
And even if we forget about the neurologic implications for a moment, you know what really bothers me? The restricted forelimb movement and blocked feeling at the base of the neck, in front of my hands and seat, was evident in my own horse even when I first started him under saddle. I just didn’t know what it was.
Likewise, one WarmbloodxTB mare had a history of treatment for neck pain dating back to three years of age, with a dressage coach clearly identifying the challenge of “always trying to get rid of that block [in the base of the neck]”, while another mare was described as “[moving] like a pony… She was 15 hands, but there was pretty much no difference between her movement and [12hh pony]’s movement.”
In my thesis, I scored each horse on the qualities of the German Training Scale, and freely admitted that the scores assigned were in all likelihood harsher than those other observers might give based on the available footage. However, this stemmed directly from the experience that what looked like a 4-5 as a bystander (and what was marked as such by judges) felt more like a 1-2 in the saddle, and this inevitably influenced my assessment of the horses I had not personally ridden.
One of the most conspicuous trends throughout the group—including those horses with more education?
The impression of biomechanical inefficiency and crude postural control, possibly attributable to dominance of and reliance on the propulsive gymnastic muscles at the expense of the proprioceptive musculature—such as the compromised m. longus colli—ordinarily responsible for refined postural adjustments.
For one TB mare, I had limited observations dating back to 2010 to work from. But you know what? I still had a very powerful impression of how rough, stiff, and unbalanced she felt to ride, and how hard it was to keep my balance on her. Fast forward roughly six years since the day I rode her myself, and my immediate impression of another TB gelding when I had the opportunity to evaluate him under saddle after nearly 18 months of observations, was the striking similarity to the mare, in spite of the huge gap.
Another interesting observation from that ride? When comparing what I was able to feel from the saddle to my bodywork findings, I was shocked to discover that the highly reactive region of muscle spasm on the right side of the gelding’s lower neck was not obvious to me when I sat on him; in fact, he was so blocked and restricted through the cervicothoracic junction that not only did this area appear immobile from above, it gave the impression of a ‘dead zone’ that I was unable to feel through the contact of my hands or seat, or influence with my aids.
Going back to my own horse, this is what I stated in the extended ridden commentary:
“I always found it difficult to maintain a balanced position when riding him, regardless of the saddle used. I felt I was constantly over-riding, especially in rising trot; it felt as if there was no rhythm or momentum to follow, and I therefore had to manufacture it by forcing myself to rise on the appropriate diagonal… I never felt like I was with him; there was no connection or flow for my body to follow and flow with.”

Echoing my personal observations of the difficulty in remaining balanced and exerting a positive postural influence when riding affected horses, the young owner of the Riding Pony mare put her struggles like this:
“I was trying to do things that I just physically couldn’t… It seemed like no matter what I did, she wouldn’t really change, and if I tried to do something, it took me a really, really long time to get it.”
When initially learning about the anomaly, I presumed that the unilaterally affected horses would seem less blocked through the cervicothoracic junction, even if their crookedness and asymmetry was marked. Likewise, I expected that even if the bilaterally affected horses were severely blocked, they would feel more symmetrical. In contrast, the bilateral horses I rode were extremely crooked, reflecting the lack of symmetry present at the skeletal level in all forms of the anomaly, and although I did not ride any of the unilaterally affected horses in the study, they visually reflected many of the blockages noted in the bilateral horses.
In all horses studied under saddle, the most severe manifestation of crookedness was characterised by deep-seated compression, contraction and torsion within the myofascial-skeletal structures of the spine, irrespective of marked deviations from the straight or curved track the horse traveled on, mild coexisting lameness, or the laterality patterns described by Dr Ridgway. This was noted as an absence of ‘throughness’ in the ridden horse, and marked by the asymmetry and functional scoliosis I found in relation to neck and DVL dysfunction.
The implication of this type of crookedness? As riders, we cannot adequately correct it using straightening aids that may work on a horse with normal anatomy and a simpler manifestation of crookedness.
The other ridden observations also underscore the malformation’s impact throughout the length of the DVL. The altered biomechanics at the cervicothoracic junction were reflected throughout its entire course, with every horse evaluated under saddle also exhibiting significant blockages through the thoracolumbar and lumbosacral regions, reducing the energy transmitted by the hindlegs even before it reached the base of the neck, with redirected or backflowing forces showing up as a visible jarring through the backs of horse and rider. This was even noted by coaches, with commentary such as “[You have to] say, ‘don’t punch my back!’”.

Biomechanically, the blockage noted at the cervicothoracic junction manifested as a disruption of the connection from the horse’s hind foot to the rider’s hand via the ring of muscles as described by Dr Deb Bennett, whereby energy generated by the hindlegs was obstructed at the level of m. longus colli’s thoracic bundle—presumably due to both the bony projection of the misplaced process into its course, and the diverted tendon fibres—thus preventing the neck telescoping gesture from completing the connection by reaching into the contact correctly.

So what can we do to help from the saddle?
Here’s my theory (and another reason for all you riders out there to learn at least a little bit about bodywork!): If we try to visualise the feel of the connection as if palpating myofascial tension via the horse-rider interface, we could better analyse the perceived blockage within the affected musculoskeletal structures, along with associated torsion.
Here’s the tough part: If we can learn to master our own postural control until we have effortless command of the structures within our human Deep Front Line, a sensitive rider could attempt to redirect the flow of energy through the horse’s DVL around the immoveable blockages and into the closest approximation of telescoping and symmetric ‘throughness’ permitted by their anatomy. This is where I suspect my early exposure to the Alexander Technique helped me sense what was going on in affected horses and, in hindsight, highly suspect horses I was riding, way before I knew anything about the malformation, and what helped me instinctively try to unwind their bodies when I started heading down the rehab path. This is not something you can achieve by force. And I really don’t have room to open Pandora’s box here, so I’ll come back to this topic in a couple of future articles.
Final thoughts…for this piece, at least
Getting back on track, one really important theme that emerged from this study was the poor clinical recognition of vertebral, postural and sensory dysfunction, even when functional problems were clearly articulated by riders, handlers, trainers or coaches. Perhaps reflecting a wider commentary on the communication between clinicians and horse owners, the stories echoed throughout this project shine a light on the metaphorical elephant of clinical examination: if an elusive physical impairment is not recognised until a sensitive and skilled trainer realises they cannot overcome the training challenges it presents, how many veterinarians are also riders with the refined feel to appreciate subtler biomechanical or proprioceptive changes and understand the rider’s concerns?
Of the remainder, how many are willing to listen thoughtfully and think laterally when a horse owner brings them a problem outside the realm of standard diagnostic criteria? While diagnostic equipment is advancing at an exponential rate, technology alone cannot distinguish between the branch and the root; nor can technology outclass the veterinarian who takes the time to piece an enigmatic clinical picture together.
To quote Haussler’s 2016 plea for a new paradigm:
“In the past, the dogma was that cervical facet osteoarthritis was the sole cause of neck pain in horses and that cervical vertebral myelopathy was the sole cause of ataxia.
Currently, we are seeing clinical cases of neck pain with little or no evidence of bony proliferation indicative of osteoarthritis on routine cervical radiographs and cases of altered proprioception and body awareness, without obvious signs of ataxia, negative myelographic findings, and no histological evidence of spinal cord compression.
This inability to readily identify subtle or poor defined causes of neck pain and altered proprioception has stimulated the need to rethink current diagnostic approaches and to expand the search into other possible sources of neck pain and dysfunction and to differentiate and localize pain syndromes within the cervicothoracic region and forelimb of affected horses.”
(Haussler, 2016, p. 1)
Amen… And I can think of a great place to start.
Coming up in Part 3….
Working With What You’re Stuck With: 5 top tips for helping horses with the Congenitally Crooked Neck…from the integrative postural rehab perspective
Disabled and doubly neurodivergent human, former equine anatomist and bodyworker (no longer practicing due to Ehlers Danlos Syndrome complications), experienced equine advocate and educator, and budding disability advocate turning my sights on Australian Government policy and practice while elevating lived experience in research for horses and humans alike.
This blog is currently inactive but I occasionally check in on Facebook. Please check out the articles I keep it alive for and take something home to your horse ❤️
Hello! I have KFS- the human equivalent of what you are describing with horses. The video is very fast (and I’m a fast reader)
Can you slow the video down a bit?
When can we expect part 3?
I used to own an extremely one sided OTTB pasture potato who only ever stood in a scissor position with his left fore forward – he was incapable of standing even so much as square for more than a couple of minutes, let alone with his right fore limb forward. I never got him ‘sound’ enough to ride as he had multiple issues (some related to his one-sidedness), but I strongly suspect that he was badly afflicted with this anomaly given his symptoms. One day I’ll dig up his skeleton to have a look.
I work with a lot of TB’s and derivatives, many of whom have at least some of the symptoms you’ve described that go along with this condition. I’m interested in learning more about assessing how ‘bad’ the condition might be based on the symptoms we see (Number of symptoms? Degree of severity?), as part of assessing the horse’s overall safety – is there some sort of checklist we could run through to say if a horse is exhibiting XYZ symptoms this indicates that further investigation is warranted to ensure that the horse isn’t a danger to itself and a rider?